

What universal healthcare should look like
The struggle to cover every American may continue for decades â€" and we need to think differently about cheap health tech and prevention first.
NOTE FOR 2021 READERS: This is the 17th in a series of award-winning open letters to the next century, now just one generation away. Kids born this year in the U.S., and nearly 50 other countries, are expected to live to 2100 and beyond. These letters examine what the world could look like then â€" and how we can make the best scenario happen.Â
Dear 22nd Century,
If you still have such a thing as a doctor's office, it might look something like the one I walked into in San Francisco the other week â€" one with no paperwork, no tablets, no visible computers at all. Instead, at a five-year-old startup called Forward Health, a doctor asked questions for nearly two hours in front of a giant touchscreen with a model of my body. We covered the interconnection of everything, from allergies to diet to workouts to that ultimate stress reducer, mindfulness. Summaries of my answers appeared on screen, not yet written by AI, but by trained medical scribes listening in remotely. At first that seemed slightly creepy, but I soon saw the point: For the first time in my medical life, a physician didn't have to spend half his time playing stenographer in a secret file. We were both on the same virtual page.
Most of my vital signs for the last decade were already on the screen when we began, since I'd granted access to my Apple Health app. My genome would follow after I downloaded the raw data from 23andMe. Analysis of a blood draw appeared in just 12 minutes; its 75 biomarkers revealed internal organs in robust good health (only my fasting glucose was a little elevated; something to keep an eye on, given a family history of diabetes). The next visit would do a deep dive on genetics; the one after that would test me for the top five most deadly cancers. In-between, there would be some gentle nudging and nagging via the Forward app, as my doctor saw new at-home readings from my Bluetooth scales or blood pressure monitor.
So yes, maybe this is a 22nd century healthcare experience. Or maybe it just looks that way because healthcare in 2021 is so far behind where it should be. Most of us are carrying around smartphones that know more about us than our doctors do, and most of our doctors don't even think to sync up with the phone data, or to get this deep into the weeds of preventative medicine. 'People walk into our exam room and go 'oh my god, I've seen the future,' says Adrian Aoun, the founder and CEO of Forward Health. 'I'm like, 'you know, they have touchscreens in McDonald's. It's just that you didn't see the past.''
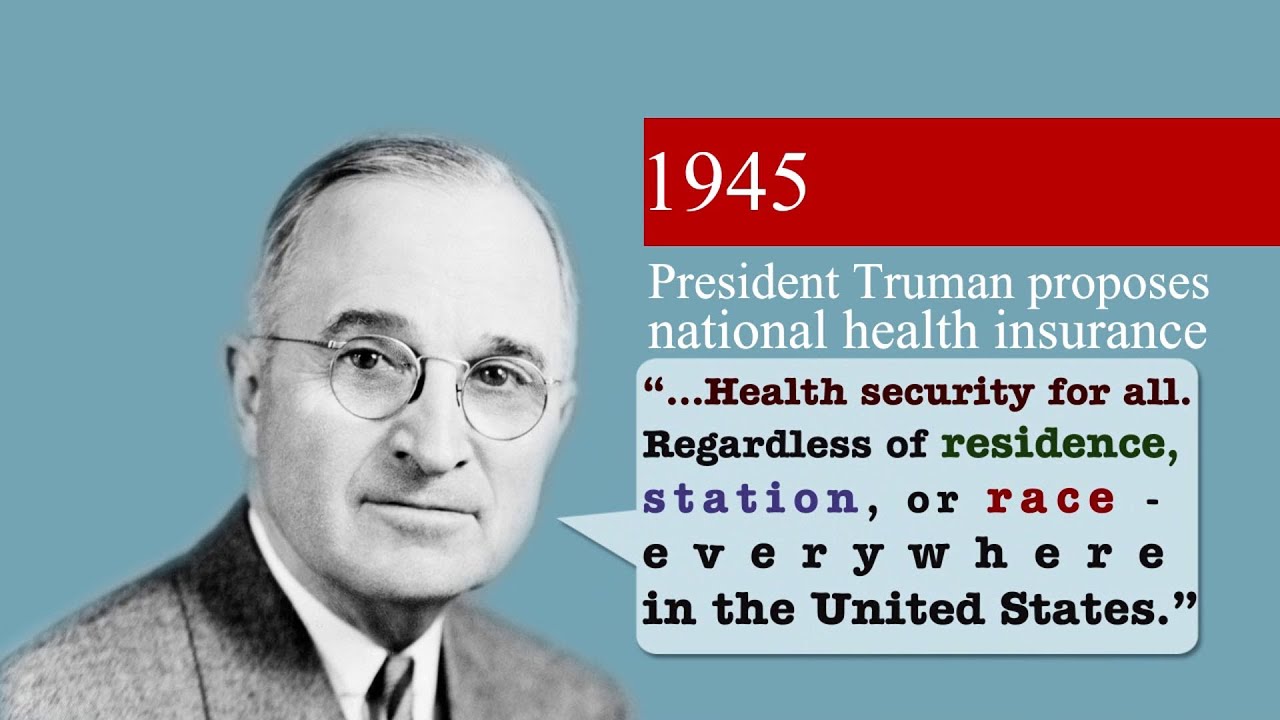
In fact, our antiquated healthcare system is such an embarrassment that I'm almost reluctant to discuss it â€" except for the fact that you may well be struggling with the same legacy problems, even eight decades hence. After all, it's been nearly eight decades since a U.S. president first tried to pass a universal healthcare law, only to run into a buzzsaw of special interests.Â
All those incremental legislative victories since, all that trench warfare against the same 'socialized medicine' boogeymen, and what have we achieved? There were more than 29 million Americans without health insurance in 2019, compared to 28 million in 2018. The COVID-19 pandemic likely threw a million more people off the insurance rolls in 2020. Medical bills are the number one reason Americans declare bankruptcy; skyrocketing premiums and deductibles, plus money-hungry for-profit hospitals, mean even the insured aren't protected from it. And as much as I adore having been born into a universal healthcare system that will bankrupt no one, the UK's beloved National Health Service (NHS), its recent underfunding and record wait times aren't much to boast about either.
But slowly, quietly, on both sides of the Atlantic, a technological revolution in preventative care is underway â€" one that may slash healthcare spending and usher in a truly universal, actually 22nd century-style wellness regime for everyone. As I wrote this letter, word came from the NHS of a breakthrough blood test that can detect relatively early signs of tumors in up to 50 cancers; I also found a UK company using the NHS' massive data sets to catch cancer development at an even earlier stage. The gene-editing technology CRISPR just casually shot down one rare disease, a foreshadowing of future victories, one perhaps against Alzheimer's. A coming wave of mRNA vaccines, buoyed by their success against COVID-19, could treat everything from malaria to various cancers (an mRNA skin cancer vaccine entered phase 2 clinical trials as I wrote this).Â
And at a more prosaic level, many of the advances we've discussed â€" more red meat replacements and indoor vegetable farms for everyone â€" cannot help but cut the body count from top killers like diabetes and heart disease.

Looked at through one lens, Forward Health seems like it could be part of the problem: It's a for-profit Silicon Valley startup with frothy amounts of funding ($225 million in its latest round, including a de rigeur celebrity investment, from The Weeknd). The 12-minute blood tests, as much as they seem to work, remind us of recent blood test-tech huckster Elizabeth Holmes. Forward's primary care services cost $149 a month, on top of any other insurance you might have, and are currently only available to the usual suspects, the well-heeled citizens of LA, New York, Chicago, SF, and Washington, D.C.Â
Those of us who worry about a two-tier 22nd century healthcare system, with a sparkling, polished, cancer-vaccinated, gene-edited elite on the one hand and a vast brink-of-bankruptcy underclass on the other, will find much to fear here.
On the other hand, maybe it's exactly the sort of company we need to help cure America's addiction to spending on sickness treatment (expected to reach $5.4 trillion, or 20 percent of U.S. GDP, in 2024). Maybe Forward and its ilk can disrupt this $11 trillion industry by being the smartphones of healthcare â€" getting the masses hooked on treating their health like a video game where the object is to have as few troubling biomarkers as possible.Â
The $149 a month cost may be expensive now (though it is the same as Medicare Part B, the government insurance we fantasize about making available to everyone, which, in addition to general medical services like diagnostics and ambulances, covers only one major preventative visit per year and one screening for the country's biggest killer, cardiovascular disease, every five years). That's the company's business plan, to keep expanding and driving down the cost and adding more services, like its new purpose-built skin cancer scanner, until the cost plummets well below monthly premiums.
'I want to keep going until Forward is as close to zero fucking dollars as possible,' says Aoun. 'That's not a joke. Not a euphemism. Literally, I would like to charge $0. And we want to keep adding value until we've built out the entire healthcare system.'
If preventative care becomes a big enough deal that it eases pressure off the hospital system, then the massive subsidies we're already spending on healthcare may be able to cover more costs. Insurance premiums, Medicare included, may plummet if they only have to cover the truly unavoidable, like accidents and rare diseases. More preventive care means fewer people on long-term drug regimens. Shorn of big payouts, Big Pharma may be forced to actually innovate again, focusing on smarter drugs and next-generation brain-stimulation tech. Maybe they can figure out how to prevent the antibiotic resistance apocalypse along the way.
It won't be all sunshine and roses, of course, because this is healthcare we're talking about: a field where 100 percent of all users die eventually, even if they make it to age 150 first. The employer-based insurance system will probably get worse before it vanishes altogether. Our employers aren't always motivated to prevent long-term health problems if you're only going to be with them for a few years on average â€" well, beyond the WW memberships and fitness trackers they offer in return for discounts on insurance costs â€" but they are motivated to peek into your genome to see if they should bother keeping you around. As laws loosen on sharing medical data, there will be some life-saving outcomes for patients; there will also be disastrous unintended consequences. The threat of genetic discrimination, like racial discrimination, looms large in many walks of life.
But if any iniquity can make a majority of the U.S. Congress finally, properly bring the health industry and its rapacious cost curve to heel, genetic discrimination will be it. By the time you arrive, 80 years in our future, Americans may finally have what we could have had for the past 80 years: Genuinely universal healthcare, prevention-focused and treated as a human right, for as close to zero fucking dollars out of pocket as possible.
A tale of two systems

FREE FOR ALL
Labour health minister Aneurin "Nye" Bevan, creator of the NHS, greets a patient in a newly nationalized hospital in 1948.
Edward G Malindine / Getty Images
In the early 21st century, honed by so much Obamacare-era combat on the issue, our attitudes to healthcare have hardened into tribal loyalties. 'Medicare for all' is the rallying cry of the Bernie Sanders-Elizabeth Warren left, who rarely stop to think about the fact that Medicare itself is too damn complicated and expensive, with giant coverage holes. (But hey, at least it won't bankrupt you.) Most opponents on the right don't defend the current system so much as spread fear with emotive, well-worn, battle-tested slogans like 'government-run healthcare' and 'socialized medicine.' So long as I live, I will never forget the cognitive dissonance of a protest sign from 2010: 'Get your damn government hands off my Medicare.'
My attitude is no less tribal. I was born and grew up in the UK, which means that like most Brits I worship at the altar of the almighty NHS, which was born from the cataclysm of World War II. As bombs fell on our cities, a government of national unity â€" Conservatives, Labour, and Liberals â€" caught the mood of the nation, which was that all this death and destruction had to be for something. We had to build a better world after the war, one in which ordinary people weren't so miserably sick of treatable diseases all the time.
'A revolutionary moment in world history is a time for revolutions, not for patching,' said the government's Beveridge Report in 1942, recommending 'comprehensive health and rehabilitation services for prevention and cure of disease' regardless of wealth. The report was a sensation. Some Conservatives tried to dampen the public's enthusiasm in the 1945 election. Prime Minister Winston Churchill himself tried socialist fearmongering; he said the Labour Party would require some kind of 'gestapo' to set up a state-run health service. A war-weary electorate wasn't buying it, and the hero of the nation lost to Labour in a landslide.
Labour health minister Aneurin Bevan established the NHS in 1948, essentially nationalizing all hospitals over Conservative objections. "No society can legitimately call itself civilized if a sick person is denied medical aid because of lack of means," Bevan famously said, and it was (and still is) hard to disagree. Ever since then, the NHS has been as popular, and politically untouchable, as Social Security in the U.S. Politicians of all stripes have competed to boast (and often lie) about how much greater they will make it, and how their opponents will destroy it. A tribute to the NHS, full of dancing nurses and whirling hospital beds, was the centerpiece of the 2012 London Olympics opening ceremony. The Brexit referendum of 2016 would not have succeeded without the Leave campaign's infamous claim that it would spend European Union membership dues on the NHS.
When I moved to the U.S. in the 1990s, the loss of the NHS was the one thing I felt most deeply. I was shocked by the amount of repetitive paperwork involved in the American system, and outraged by the cost of everything, even then. Linking healthcare and any amount of cash seemed sacrilegious, and I remember my muted rage when my first doctor's office casually requested its $10 insurance copay. Having to wait more than a day to see a GP was as alien as the free use of pharmaceutical 'samples' was sinister. I would watch Americans decry the supposed long wait times and creaking infrastructure of the UK's 'socialized medicine' and thought: Oh brother, if only you knew.

Still, as hard as it is for me to admit, the NHS is nowhere near the top of the world in many measures. In the latest ranking of global healthcare systems in the medical journal The Lancet, based on their abilities to treat and prevent a range of diseases, the UK comes in at number 23. The U.S., despite spending the most of any nation, comes in at 29. That's all I've been quibbling about, a meager six places? Most of the rest of Europe, Canada, and Australia are finding better outcomes with their single-payer healthcare systems. Scandinavian countries at the very top of the list have the benefit of great wealth (hello, Norwegian oil revenues!) and widespread acceptance of high taxes. They also boast preventative care-friendly populations that just like to eat healthier and exercise more.
That said, the NHS's COVID-19 vaccine rollout showed the advantages of this utterly centralized system over its slower single-payer brethren in the rest of Europe. All that street-level love for the NHS provides it with a large number of volunteers for various trials, which created the conditions for that 50-cancer-detecting blood test. Centralized record-keeping allows high-tech startups to come in and mine years of data for clues about which conditions (like a high blood platelet count, or elevated levels of calcium) may lead a patient to develop certain kinds of cancer in the long run.
'We're focused on a cheap and easy blood test,' says Giles Tully, CEO of a UK machine-learning company called Pinpoint Data Science that is working with the NHS to detect cancer as early as possible, and prioritize urgent cases. By the 22nd century, he says, the blood test should be able to tell you 'when your cancer is just flipping into stage 1' â€" that is, when cancerous cells have gathered into a tumor about a millimeter thick. You'll have a 'micropore' device at home, one that can poke your skin to gather blood without actually making you bleed; stick it into your smartphone and your doctor will be able to start honing in on the location of the tiny tumor. A computer-guided, highly-focused radiation treatment called a Gamma Knife could then zap the rebel cells with minimal damage to the body, and none of the side effects of expensive chemo drugs.
'The NHS has got this beautiful vision to it, and that's holding the whole damn thing together,' Tully says. 'It isn't trying to make loads of money or run the country, it's trying to stop people from dying. You need a universal system like that into which innovators can plug their cool new stuff.'
For now, though great strides are being made in preventative care, the NHS is still spending the bulk of its funding on the wrong side of the equation. British politicians' obsession with competing to build more hospitals â€" Prime Minister Boris Johnson won the 2019 election promising 40 new hospitals, another fib in itself â€" just means they're better at treating sickness than preventing it. Nobody wins elections promising to curb the nation's addictions to alcohol, crisps, chocolate, and all manner of fried fast food. 'Declines in mortality have not been matched by similar declines in morbidity, resulting in people living longer with diseases,' chides another Lancet report looking at the NHS. 'Health policies must address the causes of ill health.'
That chiding goes double for the U.S., of course. But it does mean that if and when my adopted homeland chooses to create its own NHS â€" a Department of Universal Healthcare, perhaps â€" it can create a truly futuristic system. One based on constant preventative health monitoring that molds itself around the American obsession with self-improvement. And if it helps with motivation, Americans can imagine crowing about it the moment they leapfrog those arrogant Brits in the global health rankings.
The healthcare civil war
The U.S. should have had a huge head start in preventative healthcare, given that the entire field can be summarized by one of the most famous phrases ever written by a Founding Father. An ounce of prevention is worth a pound of cure: Ben Franklin was actually talking about fire prevention, but that in itself is a great metaphor for healthcare. Just don't create the conditions for so many fires in your body. But while Americans have long accepted that government-funded fire departments are necessary for the public good, the same can not be said for government-funded healthcare.
When I first contemplated this letter, I thought it inevitable that universal healthcare would arrive in the U.S. sooner rather than later. How much longer can this country rationalize being the only developed nation in the world without any kind of national healthcare guarantee? Sure, it can take a disaster on the scale of World War II to enact that level of social change, as it did in the UK and much of Europe. 'Inequality never dies peacefully,' says historian Walter Schiedel in his sobering study of what it took to win welfare programs around the world, The Great Leveler.
Pandemics are one of the levelers Schiedel studied, and for a while it looked like COVID-19 would count as a great enough shock to the system. Surely we wouldn't have to go further down the road of likely 21st century health crises, many of them caused by a changing climate and humans encroaching on animal territory, before we figured out that this patchwork of private insurance, for-profit hospitals and overlapping agencies wasn't fit for purpose? Just as 9/11 gave us one security agency to rule them all, perhaps COVID would reveal the crying need for a Department of Universal Healthcare â€" so obviously necessary that its very acronym is DUH.
A refresher on the last 80 years of American history, and its healthcare battle Groundhog Days, soon disabused me of that notion. Even in 1945, in the wake of World War II, President Harry Truman failed to get his universal healthcare bill through a friendly Congress controlled by Democrats. The American Medical Association slammed it as â€" you guessed it â€" 'socialized medicine.'Â
The AMA compromised, if you can call it that, by backing a system of private insurance instead, which is what remains in place to this day. Twenty years later, during the liberal highwater mark of the Great Society, the best Lyndon Johnson could do was to institute Medicare and Medicaid for the elderly and needy. Which is great, but a far cry from Truman's universal coverage. And even LBJ still had to face the charge, shrieked by Cold Warriors like Ronald Reagan, that Medicare would lead to Soviet-style dictatorship.
Almost the exact same story played out at another 20-year interval, from the 1990s to the 2010s: an ambitious proposal followed by a compromise that could actually get through a Democratic Congress. First came the 1994 universal healthcare bill derided as Hillarycare, which was the reason for the first American political rally I ever attended: The Portland stop on Hillary Clinton's 1994 'Reform Riders' bus tour. The First Lady, who had agreed to start wearing a bulletproof vest after death threats, was inaudible over a crowd filled with Rush Limbaugh listeners.
I still vividly remember the guy in the Uncle Sam costume on stilts screaming 'the government's too big,' the woman standing beside me with the 'Hillary makes me sick' sign, and the reporter who came up afterwards and said, 'hi, I'm with the New York Times. Why does she make you sick?' At the time, in my naive youth, it seemed like a blip in the road to inevitable progressive victory. Now I see how much of the reactionary future was embedded in that moment.
Almost two decades after the death of Hillarycare came Obamacare, slowly and painfully compromising its way through a Democratic Congress that actually had enough senators to overcome the inevitable Republican filibuster. In a sane media landscape, the Affordable Care Act would have been widely identified as a moderate GOP proposal that originated from the conservative Heritage Foundation and was first instituted by the Republican governor of Massachusetts, Mitt Romney.
But this was the age of the Tea Party, itself misidentified as a grassroots organization rather than the Koch-brother-funded entity that historians now see it as. Fearing a Hillarycare-style debacle, President Obama preemptively abandoned the one part of the ACA that would have made the most difference, the public option: Health insurance from the government that would compete with regular insurers on the ACA marketplaces. (Even now, according to a 2020 RAND study, a public option would lower premiums by as much as 27 percent, while cutting government healthcare spending overall).

PARTY FOUL
In 2009, Tea Partiers claimed that modest improvements in the numbers of uninsured Americans would lead to "death panels."
Justin Sullivan / Getty Images
Eleven tumultuous years later, Obamacare has been watered down by a GOP Congress and president that did all they could to kill the law. A single vote from the late Sen. John McCain famously saved it from repeal. But only now in June 2021, finally, is it seen as safe after the Supreme Court declined by a 7-2 vote to give GOP states standing to challenge it.
The public option remains enormously popular, more so than Medicare For All; in multiple recent polls, as many as 70 percent of the U.S. population support the idea. As does President Biden. But with the Democrats holding the slimmest majority in the Senate, and two of their senators refusing to undo the increasingly troublesome filibuster rule that has all but brought legislation to a halt over the last 14 years, new public option legislation seems dead in the water.Â
And that's not even reckoning with the steadfast opposition of the American Hospital Association. We can't even get single-payer healthcare passed at the state level thanks to such special interests, as the latest healthcare news from the murky world of New York politics just proved.
Perhaps there will still be incremental healthcare gains in this Congress. Senate Majority Leader Chuck Schumer has just backed a Bernie Sanders plan to add dental, vision and hearing coverage to Medicare, which may be included in an upcoming infrastructure bill. To which my immediate response was: Oh for crying out loud, dental, vision, and hearing aren't already covered? Tell me again why Medicare For All should count as true universal healthcare? Biden and congressional Democrats are also pushing another popular and heartbreakingly unlikely improvement, lowering the age of Medicare eligibility from 65 to 60.
Which would chip another 1.6 million off the rolls of 30 million uninsured Americans, according to the Kaiser Family Foundation. But another analysis by consulting firm Avalere Health suggests that many of those patients would get a better deal on the ACA marketplaces than with Medicare's dizzying range of surprisingly expensive plans.
If the opportunity for truly major healthcare legislation is running on its historical schedule, we won't see another push until the 2030s â€" which itself may fail, as the 1945 and 1994 efforts did. In which case, we can expect the next Medicare/Obamacare-style incremental success (the public option, perhaps?) to pass sometime in the 2050s, then come under sustained political and legal assault in the 2060s. (Which may be when the raft of judges Donald Trump appointed to the federal bench will be in the prime of their power.)Â
Another noble healthcare law failure would be due in the 2070s, before the U.S. would be on target to finally, maybe, get a Department of Universal Healthcare across the line in the 2090s, just in time for the Americans of your era to argue endlessly about its government overreach.
Even this timeline may be too optimistic, given the GOP's current lurch towards vote-suppressing authoritarianism, QAnon irrationality, and the Democrats' dithering in the face of these threats. Which is why I reluctantly conclude that the entrepreneurs of Silicon Valley offer the best hope in the short- to mid-term of changing the healthcare landscape to our ultimate benefit.
Because if we're all going to be walking around with smartphones and smart watches anyway, we might as well use them as the foundation of a newer, healthier digital culture.
Who's going to save our health now?
Back at Forward Health, CEO Adrian Aoun certainly doesn't sound like the greatest friend that universal healthcare advocates ever had. He calls the idea that healthcare is a human right 'absurd.' He derides the NHS by insisting there's 'no way' I would move back to the UK if I needed cancer treatment. (Not true!) His role models for the company are not healthcare heroes, but Jeff Bezos and Elon Musk, both of whom constructed business models that Wall Street consistently failed to understand, for decades, until their success was assured.
But the fact that his brother had a heart attack at an early age gave Aoun religion when it comes to preventative care. 'I didn't pay attention before then,' he says. 'I was like 'I'm young, I'm healthy, I'm good to go.' And then he's there in a hospital bed, this well-to-do guy in New York City, the best doctors all surrounding him, and I'm thinking 'man, if there was just one doctor a year before telling him not to eat so goddamn much, maybe we wouldn't be here.''
Thanks to that revelation, so profoundly obvious in retrospect, Aoun's ambition doesn't just extend to remaking the entire global health industry. The food industry is an integral part of the puzzle too. 'Healthcare is not woven into what we do,' he says. 'When I walk into a restaurant, why is there not a menu personalized for my health? How have we not gotten to that level?' Indeed, we're getting closer to such a thing, now that federal law mandates fast food chains add calorie counts to menus. Perhaps by your era, more precise menus tailored to your genome and your health goals will be a thing. But in the short term, the entire $11 trillion U.S. healthcare industry will have to do as a target.
To remake it, we're all going to have to get involved. As someone who has spent the last decade increasingly obsessed with my fitness stats â€" first on Fitbit, then on Apple Watch â€" and who has used the meditation wearable Muse to launch a friendly mindfulness contest, I can confirm that the nudges involved in a regular socially-driven healthy lifestyle really do work. I suspect they'll work even more if your primary care physician is in on the action too. Training for a 5K, say, may be worth it for the plaudits you receive online from friends; it'll feel even better with your doctor enthusing about how many months you just added to your life.Â
Aoun agrees. 'Every other part of my life is continuous,' he says. 'Facebook is continuous. Why is healthcare not continuous? Why am I demanding more from my social media apps than my doctor?'
'Our traditional healthcare system is disease maintenance,' says Kevin Peake, president of LA-based Next Health, another obsessively-focused preventative primary care startup. 'Once what we do is normalized, taking part in your internal health will be like going to the gym.' Peake believes we're on the cusp of two major changes during the 2020s: Insurance companies belatedly covering more than one or two preventative care visits a year, and a new focus on the anti-aging therapies we covered in a previous letter.
To that end, Next goes a few miles further than Forward; not just looking for a larger number of micronutrients in the blood (which can slow aging and degenerative diseases) and scoping out inflammation-creating food allergies. The buzzworthy-but-still-experimental services it offers include exosomes (cellular components that may help trigger antitumor immune responses), hyperbaric oxygen therapy (which may heal some serious infections and wounds), three-minute full-body cryotherapy (super low temperatures can make your cells more resilient to everything), and potentially the most transformative tech of all, stem-cell therapy. It has a price tag to match: Next Health memberships range from $199 to $299 a month.

But this isn't just about the big, flashy, expensive, high-tech therapies. There is so much more we could be doing with our healthcare dollars in the preventative care field that we've barely even begun. Just walking briskly 30 minutes a day could cut Type II diabetes diagnoses by 50 percent, a 2016 study suggests; some insurers already offer discounts for customers who use fitness trackers, so perhaps the government could turn the same idea into an official subsidy. A 2017 study found that if just 18 percent more elementary school kids exercise for 25 minutes three times a week, their healthcare cost reductions add up to $21.9 billion over a lifetime.Â
Building more green spaces in cities, banning soda in schools, investing in anti-smoking and nutrition programs: There are proven and surprising ways to reduce the healthcare load everywhere you look, at every level of government.
One roadblock that ambitious startups like Next and Forward could run into as they expand is a shortage of primary care doctors. The Association of American Medical Colleges estimates there could be a shortfall of up to 124,000 frontline physicians by 2034. Then again, medical colleges do have a vested interest in making such a claim. Another analysis from Harvard Business Review suggests that the estimated 190,000 primary care physicians we'll have in 2025 should be enough to cover more than twice the U.S. population.
But there's no getting around the fact that physicians are drowning in paperwork, which takes roughly a third of a primary care doctor's time. Forward-style remote scribing, and increasing use of AI in medical analysis, could solve that. Another is that doctors are unevenly distributed, preferring to cluster in big cities rather than go out into the rural communities that so desperately need them. To be sure, if the COVID-19 pandemic is good for anything, it has at least normalized remote video visits. But we're going to have to work out more strategies for getting people seen for the problems that a video visit and other remote data, like that of a smartphone, can't detect.
Which would be another reason for the U.S. to adopt more of a centralized healthcare system that can manage supply and demand â€" or at least do better than a market-based system where the doctors can move to where the wealth is, but poorer patients can't just move to where the doctors are.
By the time you arrive, if you're lucky, our current healthcare system will look impossibly barbaric. Scaled-up technological solutions, multiple mRNA vaccines, a maniacal focus on preventative care, and on aging as the root cause of most suffering, plus a long-delayed DUH at the national level may improve outcomes and drive down costs to the point where you spend less on healthcare than we do. Nevertheless, I hope you continue to fight tooth and nail to reduce whatever inequality and imperfect outcomes remain lodged in the system.
Yours in good health,
2021
Read more from Dear 22nd Century
-
Written by
Chris Taylor
-
Edited by
Brittany Levine Beckman
-
Art by
Bob Al-Greene
Source : http://feeds.mashable.com/~r/Mashable/~3/VIBhLLXlIfI/universal-healthcare




No comments:
Post a Comment